Summary
Poor air quality is the largest environmental risk to public health in the UK, as long-term exposure to air pollution can cause chronic conditions such as cardiovascular and respiratory diseases as well as lung cancer, leading to reduced life expectancy.
This edition of Health matters focuses on the health impacts that air pollution can have across a person’s lifetime, the associated health inequalities, and the current and future outlook both in terms of new cases of disease and NHS and social care costs attributable to air pollution. It includes calls to action on reducing air pollution and exposure for the health service and healthcare professionals, local government, and the public.
Scale of the problem
Air pollution has a significant effect on public health, and poor air quality is the largest environmental risk to public health in the UK. In 2010, the Environment Audit Committee considered that the cost of health impacts of air pollution was likely to exceed estimates of £8 to 20 billion.
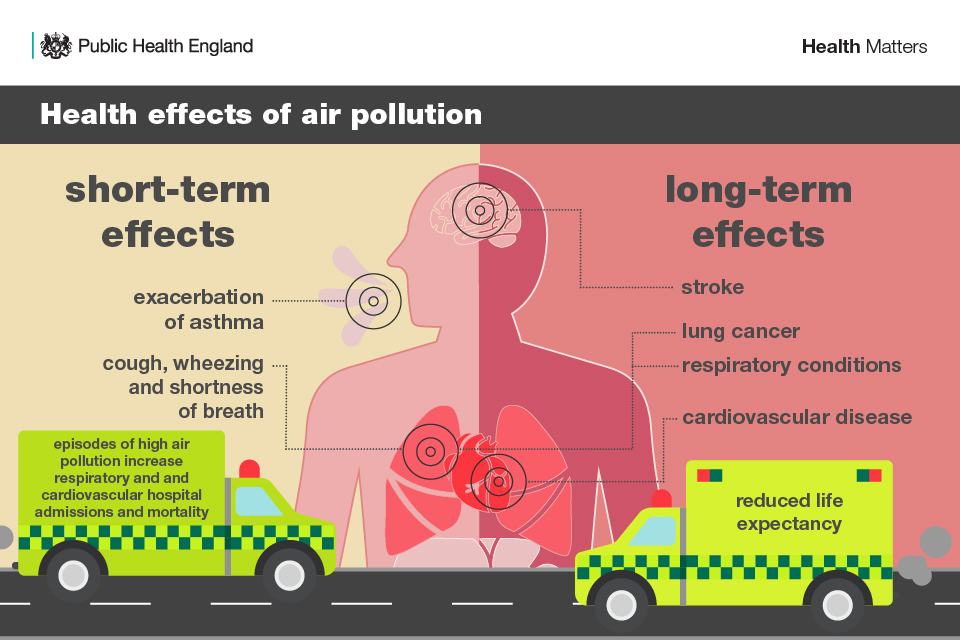
Epidemiological studies have shown that long-term exposure to air pollution (over years or lifetimes) reduces life expectancy, mainly due to cardiovascular and respiratory diseases and lung cancer. Short-term exposure (over hours or days) to elevated levels of air pollution can also cause a range of health impacts, including effects on lung function, exacerbation of asthma, increases in respiratory and cardiovascular hospital admissions and mortality.
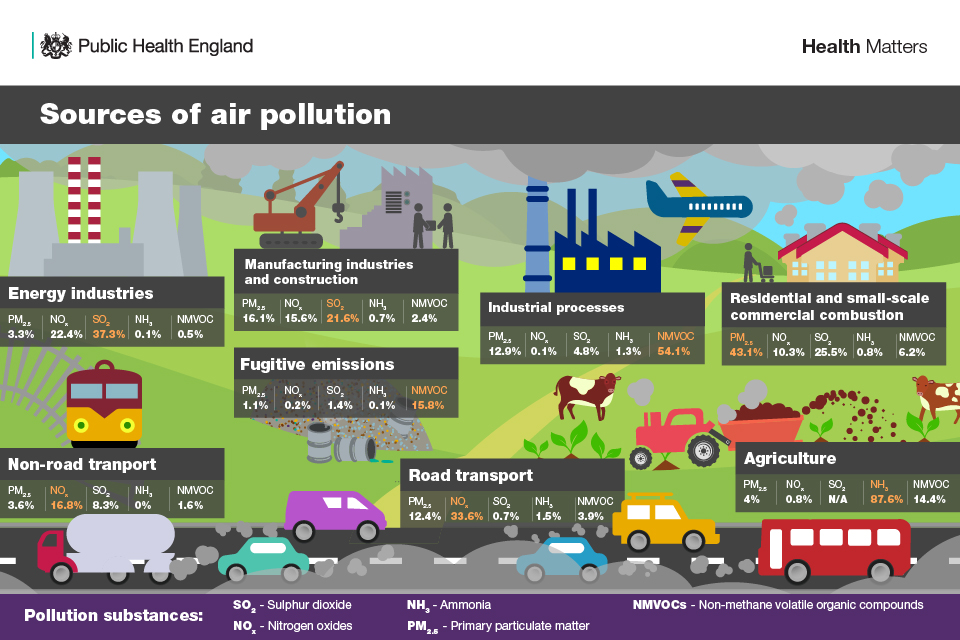
Air pollutants are emitted from a range of both man-made and natural sources. Many everyday activities such as transport, industrial processes, farming, energy generation and domestic heating can have a detrimental effect on air quality.
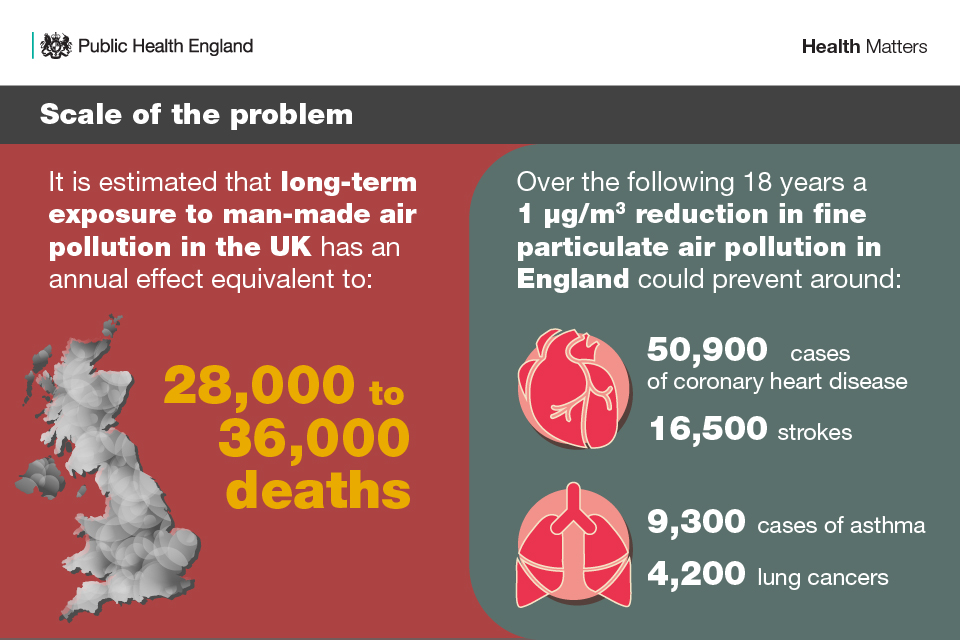
The UK Health Forum and Imperial College London, in collaboration with and funded by Public Health England (PHE), developed a modelling framework and estimated that a 1 µg/m3 reduction in fine particulate air pollution in England could prevent around 50,900 cases of coronary heart disease, 16,500 strokes, 9,300 cases of asthma and 4,200 lung cancers over an 18 year period.
There are legal requirements and aspirational targets for levels of different air pollutants. The government recognises that protective health – and tackling air pollution – requires action, and is committed to improving the UK’s air quality and reducing harmful emissions. The draft Clean Air Strategy, published in May 2018, sets out the case for action and demonstrates the government’s determination to improve our air quality.
The key air pollutants
Air pollution is a complex mix of particles and gases of both natural and human origin. Particulate matter (PM) and nitrogen dioxide (NO2) are both major components of urban air pollution. Currently, there is no clear evidence of a safe level of exposure below which there is no risk of adverse health effects. Therefore, further reduction of PM or NO2 concentrations below air quality standards is likely to bring additional health benefits.
1. Particulate matter (PM)
PM is a generic term used to describe a complex mixture of solid and liquid particles of varying size, shape, and composition. Some particles are emitted directly (primary PM); others are formed in the atmosphere through complex chemical reactions (secondary PM). The composition of PM varies greatly and depends on many factors, such as geographical location, emission sources and weather.
The main sources of man-made PM are the combustion of fuels (by vehicles, industry and domestic properties) and other physical processes such as tyre and brake wear. Natural sources include wind-blown soil and dust, sea spray particles, and fires involving burning vegetation.
PM is often classified according to by aerodynamic size and referred to as:
- coarse particles (PM10; particles that are less than 10 microns (µm) in diameter)
- fine particles (PM2.5; particles that are less than 2.5 µm in diameter)
- ultrafine particles (PM0.1; particles that are less than 0.1 µm in diameter)
The size of particles and the duration of exposure are key determinants of potential adverse health effects. Particles larger than 10 µm are mainly deposited in the nose or throat, whereas particles smaller than 10 µm pose the greatest risk because they can be drawn deeper into the lung. The strongest evidence for effects on health is associated with fine particles (PM2.5).
There is an extensive body of evidence that long-term exposure to PM increases mortality and morbidity from cardiovascular and respiratory diseases. Outdoor air pollution, particularly PM, has also been classified by the International Agency for Research on Cancer (IARC) as carcinogenic to humans (a Group 1 carcinogen) and causing lung cancer. There is some experimental evidence, however, that ultrafine particles may also pass through the lungs into the bloodstream.
2. Nitrogen dioxide (NO2)
NO2 is a gas that is produced along with nitric oxide (NO) by combustion processes. Together they are often referred to as oxides of nitrogen (NOx).
The Department for Environment, Food & Rural Affairs (Defra) estimates that 80% of NOx emissions in areas where the UK is exceeding NO2 limits are due to transport, with the largest source being emissions from diesel light duty vehicles (cars and vans). Other sources include power generation, industrial processes, and domestic heating.
The Committee on the Medical Effects of Air Pollutants (COMEAP) has established that short-term exposure to NO2, particularly at high concentrations, is a respiratory irritant that can cause inflammation of the airways leading to – for example – cough, production of mucus and shortness of breath. Studies have shown associations of NO2 in outdoor air with reduced lung development, and respiratory infections in early childhood and effects on lung function in adulthood.
Epidemiological studies have also shown associations of outdoor NO2 with adverse effects on health, including reduced life expectancy. It has been unclear whether these effects are caused by NO2 itself, or by other pollutants emitted at the same time by sources such as road traffic.
3. Other pollutants
3.1 . Sulphur dioxide (SO2)
SO2 is produced when sulphur-containing fuels, such as coal, are burned. It is an invisible gas with a sharp smell and can dissolve in water. Chemical reactions of SO2 can also produce sulphates, which remain in the air as secondary particles, contributing to the PM mix.
SO2 has an irritant effect on the lining of the nose, throat and airways, and the effects are often felt very quickly. Due to the increased use of gas and electricity, coal-burning is now relatively uncommon, and levels of SO2 have steadily declined over the last 50 years. Most SO2 in the UK now comes from industrial sources, such as coal and oil-burning power stations, as well as domestic sources such as boilers and stoves.
3.2 . Ammonia (NH3)
NH3 is a gas released into the atmosphere from natural and man-made sources. Once emitted into the atmosphere, the subsequent deposition of NH3 can be a major source of pollution, causing nitrogen (N) enrichment (eutrophication) and acidification of soil and water sources. Atmospheric NH3 also reacts with acid gases, such as sulphuric and nitric acid, to form secondary PM2.5.
The main health impacts of NH3 arise through its role in secondary PM2.5 formation and health effects associated with exposure to PM, as described above. Thus, NH3 not only plays a role in acidification and eutrophication but also contributes to the overall PM burden. Agricultural emissions of NH3 have been reported to be key contributor to some short-term episodes of high PM pollution in recent years.
3.3 . Ozone (O3)
O3 is a gas and occurs both in the earth’s upper atmosphere and at ground level. Ground level, or tropospheric O3, is not emitted directly into the air but is created by photochemical reactions involving the precursor pollutants NOx and volatile organic compounds (VOCs). Several epidemiological studies have reported adverse associations between short-term exposure to O3 and human health.
The effects of exposure to O3 are predominantly respiratory, but adverse effects on the cardiovascular system have also been reported. Less convincing evidence exists for an association between long-term exposure to O3 and impacts on human health.
3.4 . Carbon monoxide (CO)
CO is a colourless, odourless and tasteless gas, produced when fuels such as gas, oil, coal and wood burn without enough oxygen. These are sources of fuel used in many household appliances, including boilers, central heating systems, gas fires, water heaters, cookers and open fires. Burning charcoal, running cars and the smoke from cigarettes also produce CO gas. Exposure to high indoor levels can be fatal, while exposure to lower levels can result in symptoms that resemble flu, viral infections or food poisoning.
More information about CO in this collection and on the NHS website.
3.5 . Non-Methane Volatile Organic Compounds (NMVOCs)
NMVOCs consist of a large variety of chemically different compounds and in the environment come from both natural and anthropogenic sources. The total anthropogenic NMVOC emissions in the UK have decreased by 68% between 1970 and 2016. The rate of decline was most pronounced in the 1990s, largely reflecting the decline in coal mining, and has slowed in recent years. NMVOCs are emitted from a wide variety of products and processes including industrial processes and agriculture, and they also form a significant component of indoor air pollution emitted from household products.
In the outside atmosphere, NMVOCs react with NOx in the presence of sunlight to form tropospheric O3, known to be harmful to health and the environment.
Indoors, VOCs emitted from consumer products are not thought be to a significant public health issue when homes are well ventilated and when the products are used according to the manufacturers’ instructions. But some sensitive people may suffer irritation of the eyes, nose and throat, headaches and dizziness if they are exposed.
Indoor air pollution
Air pollution isn’t just about the outdoor world. There are a number of sources of indoor air pollutants that can harm health including:
- CO, NO2 and particulates from domestic appliances (boilers, heaters, fires, stoves and ovens), which burn carbon containing fuels (coal, coke, gas, kerosene and wood)
- VOCs from cleaning and personal care products, building materials and household consumer products (paints, carpets, laminate furniture, cleaning products, air fresheners, polishing)
- environmental tobacco smoke (ETS) and second hand smoke (SHS)
- radon is a naturally occurring radioactive gas that comes from the ground as the earth decays. There is an increased risk of lung cancer if exposed to high levels of radon for a long time, as it is the second highest cause of lung cancer after smoking. It’s generally not a problem in outside air but can accumulate in buildings.
PHE works with government and others to develop and review the evidence on indoor air quality. This includes the Royal College of Physicians and Royal College of Paediatrics and Child Health’s systematic review on the effects of Indoor Air Quality on Children and Young People’s Health.
Why invest?
PHE’s cost of air pollution project quantified the potential costs to the NHS and social care system due to the health impacts of PM2.5 and NO2 in England. It estimated that between 2017 and 2025, the total cost of air pollutants for which there was more robust evidence for an association, was £1.69 billion for PM2.5 and NO2 combined (£1.54 billion for PM2.5 and £60.81 million for NO2). A tool to estimate the cost of air pollution for each local authority was made available, as part of this project.
Air pollution can impact people of working age, which can also have economic effects, for instance, if they have to take days off work. Defra estimated that in 2012, poor air quality cost the economy £2.7 billion through its impact on productivity.
Dealing with poor air quality in all its forms is a priority for the government, with the UK having signed up to tougher legally binding national emission ceilings for 5 major pollutants (PM, NO2, SO2, NMVOCs and NH3). In the draft Clean Air Strategy, the government has committed to reducing the harm to human health from air pollution by halving the population living in areas with concentrations of fine PM above World Health Organization (WHO) guideline levels (10µg/m3) by 2025.
Air pollution is not an issue that occurs in isolation. Pollution can be associated with other environmental hazards that affect health, and it can contribute to health inequalities. However, measures that improve air quality can also offer wider public health and wellbeing co-benefits, including an improvement in overall environmental quality, increased physical activity, noise reduction, greater road safety and climate change mitigation. Multiple interventions, each producing a small benefit, can act cumulatively to produce significant overall benefits.
How air pollution harms health
1. Where pollutants go in the body and what they do
When air pollutants enter the body, they can have effects on various different organs and systems, not just the respiratory system.
This includes:
- the eyes, nose and throat
- the lungs and respiratory system
- the heart – heart and blood vessel diseases, including strokes and hardening of the arteries, are one of the main effects of air pollution
Emerging evidence suggests that air pollution may also affect the brain and is possibly linked to dementia and cognitive decline. There is also emerging evidence associating air pollution with early life effects such as low birth weight.
2. Impact of air pollution across a person’s lifetime
Air pollution can affect everyone, and air in all areas of the UK contains some proportion of man-made air pollutants. Exposure to air pollution has various different health effects, which come about at every stage of life, from a foetus’ first weeks in the womb all the way through to old age. The health effects of air pollution are complex, and range in severity of impact. In some cases, damage can be gradual and may not become apparent for many years.
The 3 main conditions associated with air pollution are respiratory conditions (such as asthma), cardiovascular disease (CVD), and lung cancer, and there is emerging evidence for associations with dementia, low birth weight and Type 2 diabetes. COMEAP has highlighted that exposure to air pollution contributes to many thousands of deaths in the UK, through increasing the risk of CVD, respiratory disease and cancers.
There is therefore a strong case for action to tackle air pollution, and action to improve air quality and health is a priority area for PHE.
The following sections outline the various health effects and conditions that come about at different stages of life. The Royal College of Physicians’ report, ‘Every breath we take: The lifelong impact of air pollution’, presents the findings of multiple international studies regarding each of these health effects.
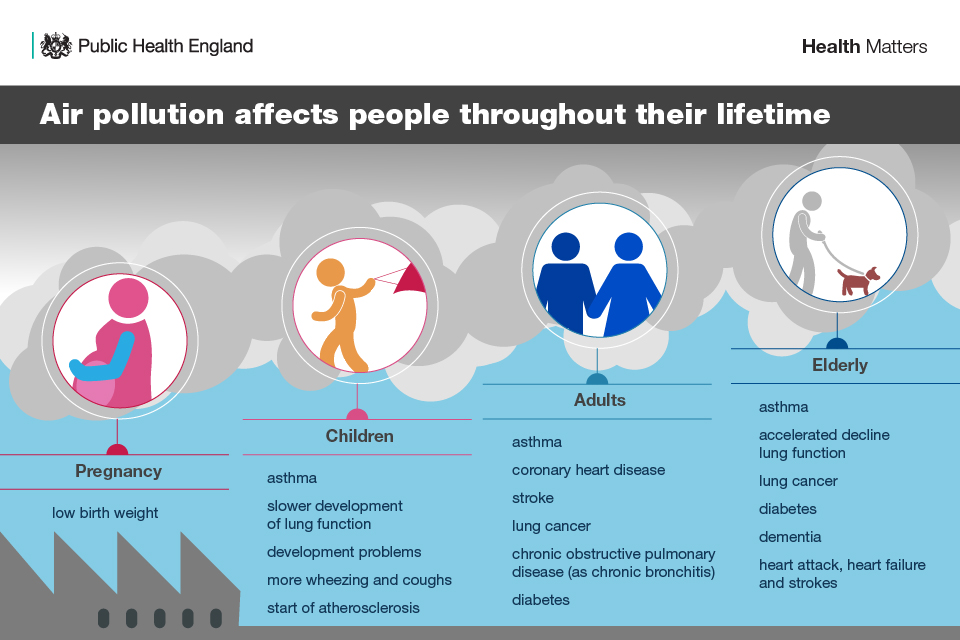
2.1 . Early childhood development: pregnancy, the developing foetus and infancy
Pregnancy and early childhood are critical times for the formation and maturation of body systems, and the time during which the most rapid changes take place. Factors that adversely affect human development, including air pollution, can have both immediate and long-lasting effects on a person’s health, and some health impacts may only emerge later in life.
As well as potential effects on foetal growth, air pollution exposure is associated with low birth weight and premature birth.
2.2 . Lung function development and decline
Exposure to air pollution in early life can have a long-lasting effect on lung function. There is evidence that the process of normal lung function growth in children is suppressed by long-term exposure to air pollution. Throughout childhood, there is a natural development of lung function and maximising this is important, as low lung function leads to less reserve if lung disease develops.
Lung function in adulthood slowly declines with age, and there is emerging evidence that air pollution and living near a busy road accelerate this decline, for both adults and older people. Minimising this is important to maximise reserve, especially if lung disease develops in later life.
2.3 . Asthma
Asthma, a long-term inflammatory condition of the conducting airways of the lungs, leads to cough, wheezing, chest tightness, and shortness of breath. Asthma symptoms in those who have the condition can be exacerbated by various stressors, including respiratory viral infection, allergen exposure, and episodes of elevated air pollution.
There is increasing evidence of air pollution having a potential role in causing asthma, especially in people who live near busy roads, as well as being a trigger that can make an asthmatic’s symptoms worse.
2.4 . Cardiovascular disease
There is strong evidence for the effects of both short and long-term exposures to air pollution on CVD in adults. Air pollution can both contribute to the development of CVD and exacerbate heart conditions that already exist, with the strongest associations having been observed for PM. The COMEAP report: The Effects of Long-Term Exposure to Ambient Air Pollution on Cardiovascular Morbidity: Mechanistic Evidence, details the mechanisms of effect of air pollutants as they impact on cardiovascular morbidity.
The risk of heart failure, myocardial infarction (heart attacks), arrhythmias (abnormal rhythms of the heart) and stroke is increased by both short and long-term exposure to air pollution in susceptible individuals. This includes older people and individuals with pre-existing cardiovascular and respiratory conditions. The strongest associations have been observed for fine PM, which is associated with both cardiovascular morbidity and a reduction in life expectancy as a result of increased death from CVD (and respiratory disease and lung cancer).
Despite the robust evidence for adults, it remains unclear whether exposure to air pollution during childhood influences CVD development in later life. However, it has been found that in children, there are changes in biomarkers of cardiovascular function, such as blood pressure and pulmonary arterial pressure, after exposure to air pollution.
2.5 . Cancer
There is strong evidence that outdoor air pollution is linked to lung cancer, and the IARC has classified outdoor air pollution and PM from outdoor air pollution as carcinogenic to humans.
Despite the strong evidence for adults, there is weaker evidence related to effects on children, with the World Health Organization (WHO) reporting in 2005 that there was ‘insufficient evidence for ambient air pollution and childhood cancer’. This could be in part due to lung cancer being rare in children. However, as it is believed that lung cancer can take many years to develop following exposure, some research suggests that exposure in childhood could contribute to the development of cancers in later life.
3. Current and future impact
Having a thorough understanding of how air pollution is likely to impact health and related healthcare costs over time is important for future policy and resource planning. The Environmental Audit Committee has estimated that health costs as a result of air pollution range between £8.5 billion and £20.2 billion a year.
To estimate the NHS and social care costs for treating health effects, PHE developed a modelling framework to quantify present and future morbidity. PHE’s report, Estimation of costs to the NHS and social care due to the health impacts of air pollution, provides the methods and results of the modelling exercise to quantify:
- the future incidence and cumulative incidence cases of air pollution related diseases
- the NHS and social care costs; specifically primary care, prescription, secondary care, and social care, associated with air pollution
The following sections present the incidence of all conditions associated with long-term exposure to PM2.5 and NO2 in England, as quantified by the modelling framework. It makes a strong case for investing in prevention and early intervention at local and national levels, as well as allowing the necessary resources for the cases that cannot be prevented.
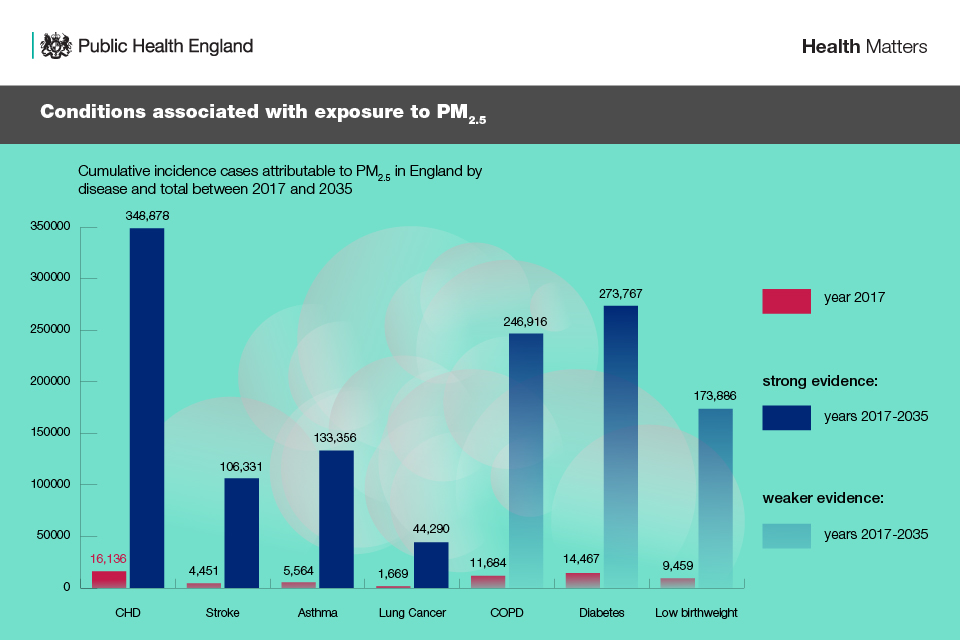
3.1 . Conditions associated with exposure to PM2.5
As presented in the table below, PHE’s modelling framework found that in 2017 there were 63,430 (±2,154) total incidence cases of disease attributable to PM2.5 in England.
It is predicted that between 2017 and 2035, 1,327,424 (±9,927) new cases of disease would be attributable to PM2.5, equivalent to 2,248 new cases of disease per 100,000 people. The highest numbers of these cases are predicted to be from coronary heart disease (CHD), diabetes and COPD.
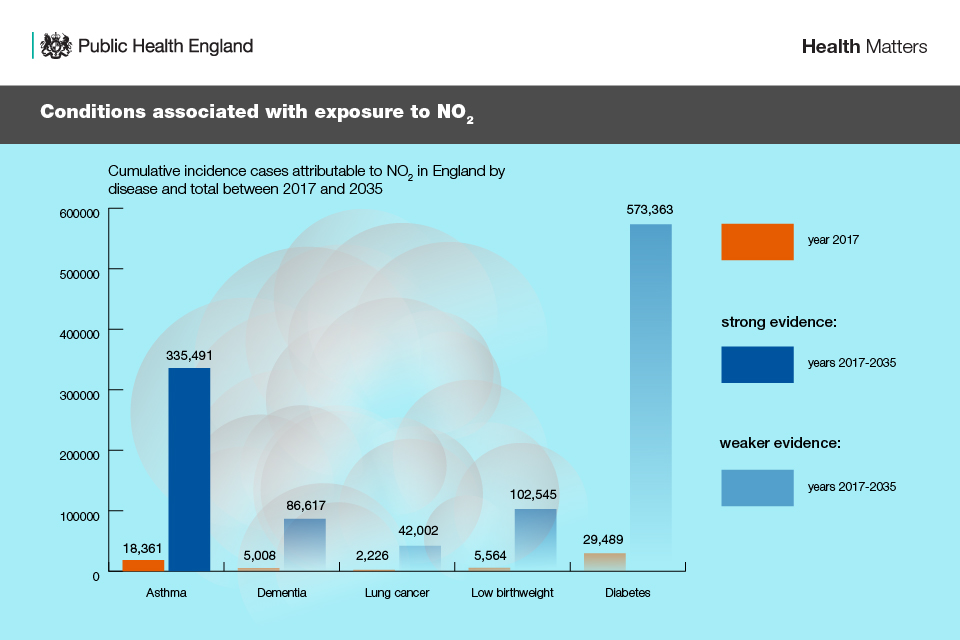
3.2 . Conditions associated with exposure to NO2
PHE’s modelling framework found that in 2017, there were 60,648 (±2,549) total incidence cases of disease attributable to NO2 in England. It is predicted that between 2017 and 2035, 1,140,018 (±11,800) new cases of disease would be attributable to NO2, equivalent to 1,933 new cases of disease per 100,000 people. The highest numbers of these cases are predicted to be from diabetes and asthma.
4. Air pollution and health inequalities
Although air pollution can be harmful to everyone, some people are more affected because they live in a polluted area, are exposed to higher levels of air pollution in their day-to-day lives, or are more susceptible to health problems caused by air pollution. The most vulnerable face all of these disadvantages.
Groups that are more affected by air pollution include:
- older people
- children
- individuals with existing CVD or respiratory disease
- pregnant women
- communities in areas of higher pollution, such as close to busy roads
- low-income communities
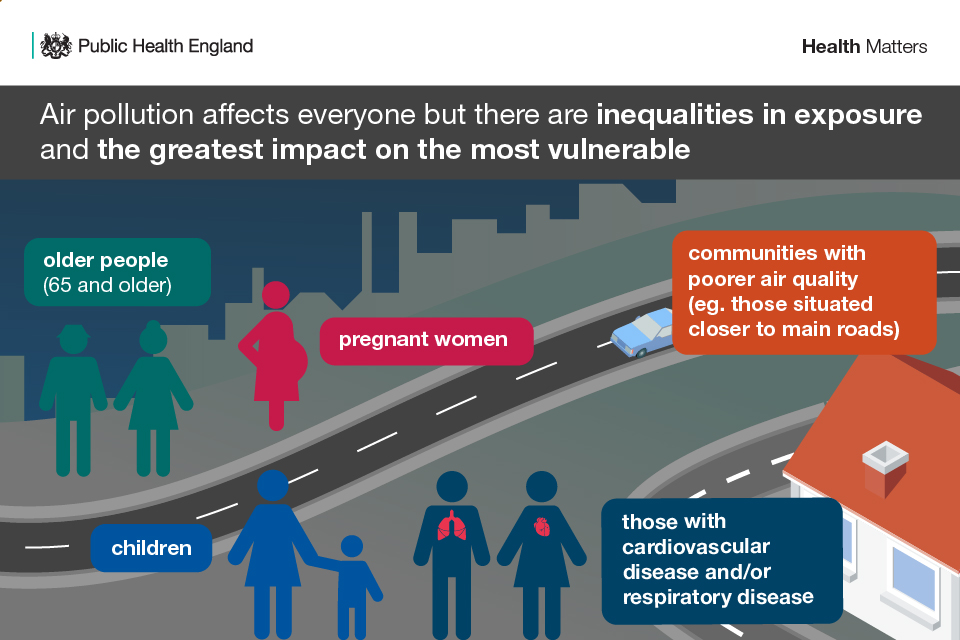
4.1 . Low-income communities
There is clear evidence that people with a low income are affected by air pollution in a number of different ways.
This is because they are more likely to:
- have existing medical conditions
- live in areas with poorer outdoor and indoor environments, including the quality of air (for example, near to industry or busy roads)
- have less access to jobs, healthy food, decent housing and green spaces, which all contribute to poorer health
The disadvantages that come about as a result of poor income add up, putting deprived populations who are more likely to be in poor health at greater risk from air pollution and its adverse health impacts. These inequalities can also affect people throughout their lives, from the prenatal stage through to old age, particularly as deprived communities often have limited opportunities to improve their environment.
Call to action: reducing air pollution
Improving air quality is crucial to reduce the health impacts discussed above and, in turn, help people live longer, healthier lives. A study in 2006 found that reducing PM by 10µg/m3 would extend lifespan in the UK by 5 times more than eliminating casualties on the roads, or 3 times more than eliminating passive smoking.
Everyone needs to play their part.
Local government
Local authorities have a statutory role in assessing and improving local air quality, and the cumulative effects of this local action are significant. The effect of a range of interventions to improve air quality has greater potential to reduce the associated burden of disease than anyone intervention alone. As the greatest impact will be achieved by synergistic packages of interventions, a strategic approach involving a combination of legislative, policy, behavioural and technological interventions is required in order to realise the greatest benefits.
When new plans and programmes are designed, and when new development or regulatory consents are issued, options appraisals can preferentially select approaches that have the greatest potential to benefit air quality and health.
PHE recommends that evaluation is embedded in the design and costing of all future national and local interventions, from their outset, to systematically gather evidence of effectiveness and cost-effectiveness to inform future policy development.
Councils can:
- invest in infrastructure and public transport, and promote active travel and cycle routes
- implement measures to reduce air pollution caused by road traffic and other sources
- design healthy environments, bringing in spatial planning, urban design, road and building layouts, and green spaces